On November 9th, 2023, Hope Roots hosted a 1-hour Free Discussion with Dorinna Ruh with tools to help therapists learn to assess clients for dissociation. This call, and other training resources are provided as part of Hope Roots' mission to increase access to trauma-informed care. For more resources like this, please subscribe on YouTube at https://www.youtube.com/@hoperoots and signup for email updates when new resources are posted.
Event Description
Discovering a client’s dissociative disorder is the first step toward their receiving proper treatment. Yet many therapists do not get adequate training regarding dissociation, specifically how to assess it. As a result, it takes between 5 - 12 years for someone in therapy to get diagnosed with a dissociative disorder (Brand BL, Loewenstein RJ, Spiegel D. Dispelling myths about dissociative identity disorder treatment: an empirically based approach. Psychiatry. 2014 Summer;77(2):169-89).
Dorinna Ruh has taught advanced EMDR Therapy skills since 2010 as an EMDRIA-approved consultant and specializes in dissociative disorders. Learn more about Dorinna’s work at https://advanced-emdr-education.com/ In this free call, Dorinna will review dissociation assessment for therapists who want to ensure they have the basic skills needed to identify clients who may have a dissociative disorder. No CEUs will be given.
Donations Appreciated
If you find this offering of value, please consider sending a donation to Hope Roots, so we can continue our mission of increasing access to trauma-informed care (including training opportunities like this!). You can also Venmo a donation (@hoperoots).
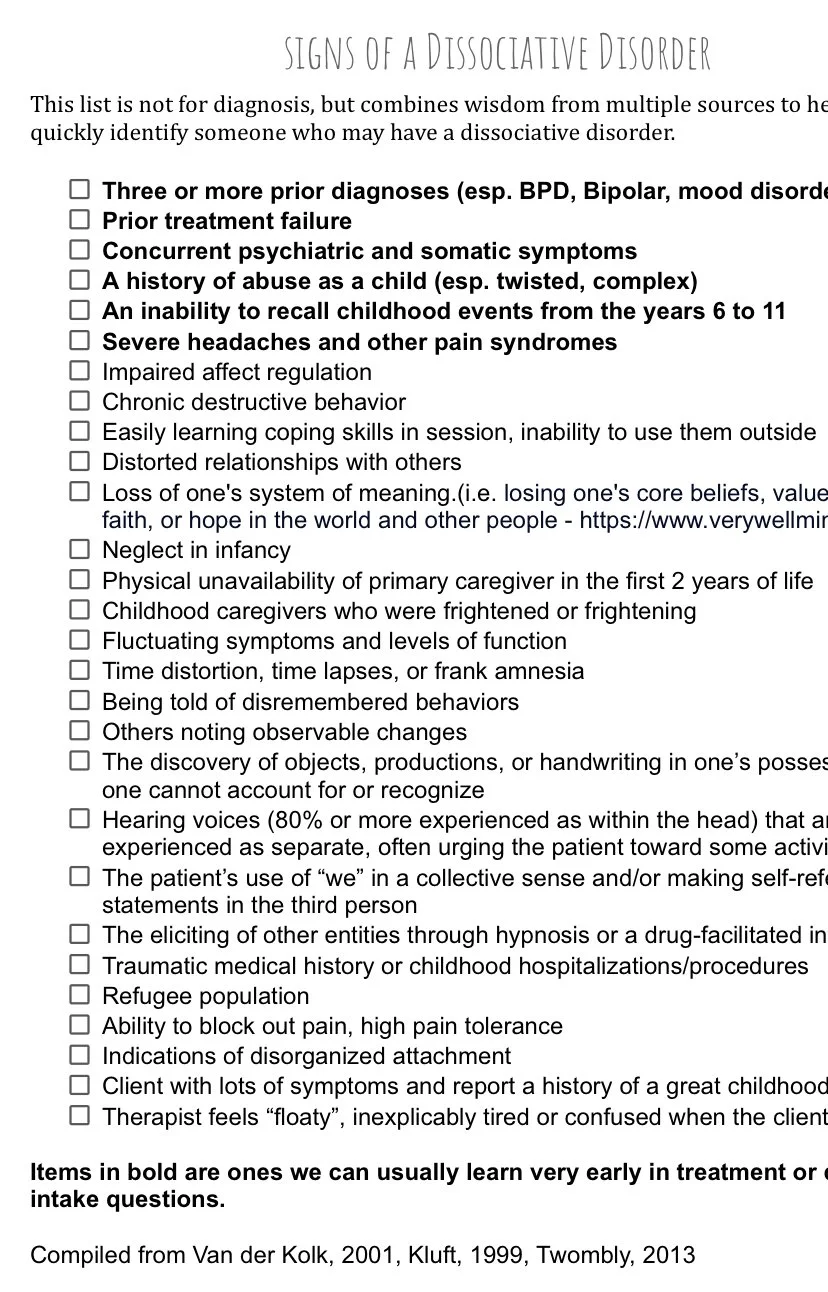
This list is not for diagnosis, but combines wisdom from multiple sources to help trauma therapists more quickly identify someone who may have a dissociative disorder. Click here to download a PDF of this handout.
Three or more prior diagnoses (esp. BPD, Bipolar, mood disorders)
Prior treatment failure
Concurrent psychiatric and somatic symptoms
A history of abuse as a child (esp. twisted, complex)
An inability to recall childhood events from the years 6 to 11
Severe headaches and other pain syndromes
Impaired affect regulation
Chronic destructive behavior
Easily learning coping skills in session, inability to use them outside
Distorted relationships with others
Loss of one's system of meaning.(i.e. losing one's core beliefs, values, religious faith, or hope in the world and other people - https://www.verywellmind.com)
Neglect in infancy
Physical unavailability of primary caregiver in the first 2 years of life
Childhood caregivers who were frightened or frightening
Fluctuating symptoms and levels of function
Time distortion, time lapses, or frank amnesia
Being told of disremembered behaviors
Others noting observable changes
The discovery of objects, productions, or handwriting in one’s possession that one cannot account for or recognize
Hearing voices (80% or more experienced as within the head) that are experienced as separate, often urging the patient toward some activity
The patient’s use of “we” in a collective sense and/or making self-referential statements in the third person
The eliciting of other entities through hypnosis or a drug-facilitated interview
Traumatic medical history or childhood hospitalizations/procedures
Refugee population
Ability to block out pain, high pain tolerance Indications of disorganized attachment
Client with lots of symptoms and report a history of a great childhood
Therapist feels “floaty”, inexplicably tired or confused when the client is present .
Items in bold are ones we can usually learn very early in treatment or during intake questions
Compiled from Van der Kolk, 2001, Kluft, 1999, Twombly, 2013
In EMDR Therapy, clients reprocess not just a single traumatic memory, but any past memories and present triggers that are fueling their present symptoms. For instance, if the presenting problem is social anxiety the clinician will help the client explore the present triggers related to their symptoms (i.e. the grocery store is crowded) and then use a “floatback” technique to make a list of past memories that are connected to those thoughts, emotions, and sensations in the client’s memory network (i.e. age 5 - lost in store; age 27 - robbery). The client will also consider how they will feel and respond in the future after EMDR therapy (i.e. a calm trip to the store). An EMDR Therapy treatment plan is completed when a client has reprocessed any past memories, any present triggers, and can visualize themselves successfully navigating the future without distress. The worksheet below can be used by EMDR-trained clinicians to map out a plan for a client’s EMDR therapy.
Our go-to resources for clients who are learning mindfulness and grounding skills in preparation for trauma therapy or have begun their trauma work and are ready to listen more to their bodies and practice calm awareness. These tools are ideal for anyone who deals with stress (so, everyone).
Count Your Breathing with a Ratio
There are many great breathing exercises, but my favorite go-to for grounding with the breath is inhaling for 4 counts, then exhaling for 4 counts; then inhaling for 5 counts, and exhaling for 5 counts. Continue adding a count until you get up to inhaling for a count of 8 and exhaling for a count of 8 (4:4,5:5,6:6,7:7,8:8). The great thing about this one is that you can do it anywhere. No one will know you are counting in your head and your breaths don’t have to be particularly deep. The practice of making the exhale the same length as the inhale and then lengthening the breaths will usually bring calm. The added cognitive effort of counting is helpful too and requires you to bring other parts of your brain online that may have been stuck in a stress/survival mode. There are other breathing exercises that involve counting, or ratio breathing. Often there are three numbers, with the middle number being how many counts to hold your breath in between the inhale and the exhale. A common ratio is 4:7:8, but there are many combinations. I typically avoid cueing breath retention when working with trauma survivors but feel free to explore how your system responds to different ratios.
Count Colors & Find your Senses
When a client in my office needs help feeling more present the first thing I typically say is, “How many shades of green can you count in this room?” (Hint: it’s a ridiculous amount due to all the plants). As they begin to look around and count, they usually feel calmer and more present in just a few seconds. Sometimes they laugh and say, “That is really a lot of greens!”. You can build onto this tool by then noticing what you can touch or hear. One way to incorporate both counting and noticing present safety (Note: every one of your senses can work as an alarm for your nervous system) is with a 5-4-3-2-1 grounding exercise. Find 5 things you can see, then 4 things you can touch, 3 things you can hear, 2 things you can smell, and 1 thing you can touch. If you can’t remember which number goes with each sense just start with looking or feeling around you for anything interesting then check in with all of your senses.
Find the Ground
Okay, the most obvious “grounding” tool is simply to notice the ground beneath you. Notice every part of you that is connected to the ground (sofa, yoga mat, sidewalk, car seat, floor) beneath you. If your feet are on the ground, wiggle your toes and notice all of the parts of your feet that are touching the floor… roll forward onto the balls of your feet or back onto your heels. What feels calm or peaceful about being where you are right now? If you are sitting or lying down, notice every part of you that can touch what is beneath you. Imagine that your body is like a sandbag and move slightly, imagining how the sand shifts. What is good about being present here at this moment?
The Wheel of Awareness from Dr. Dan Siegel
https://drdansiegel.com/wheel-of-awareness/
Dr. Dan Siegel has spent years researching and helping clients using mindfulness practices and integration. The Wheel of Awareness is a practice that helps us train our brains to shift awareness, notice what is happening in and around us with mindful awareness, and ultimately find solace in pulling away from all that we can be aware of by being in the “Hub”. The link above contains Dr. Siegel’s diagram showing the “Wheel of Awareness” followed by several links to guided audio meditations and teachings about the Wheel. If you have time, try the full 30-minute version or the basic 20-minute version. If not, try the consolidated 7-minute version. Disclaimer: Mindfulness is hard. It’s supposed to be challenging. It gets easier the more you practice it (like most things). So, go easy on yourself and make a plan to try it again soon. Trauma warning: The longer versions of the Wheel cue the listener to notice the body in very detailed ways (organs, specific areas of the body). This very-detailed level of body awareness can be triggering for some individuals. If you find that’s true for you, feel free to skip the “cues to notice” that are triggering and explore those triggers in individual therapy when you are ready.
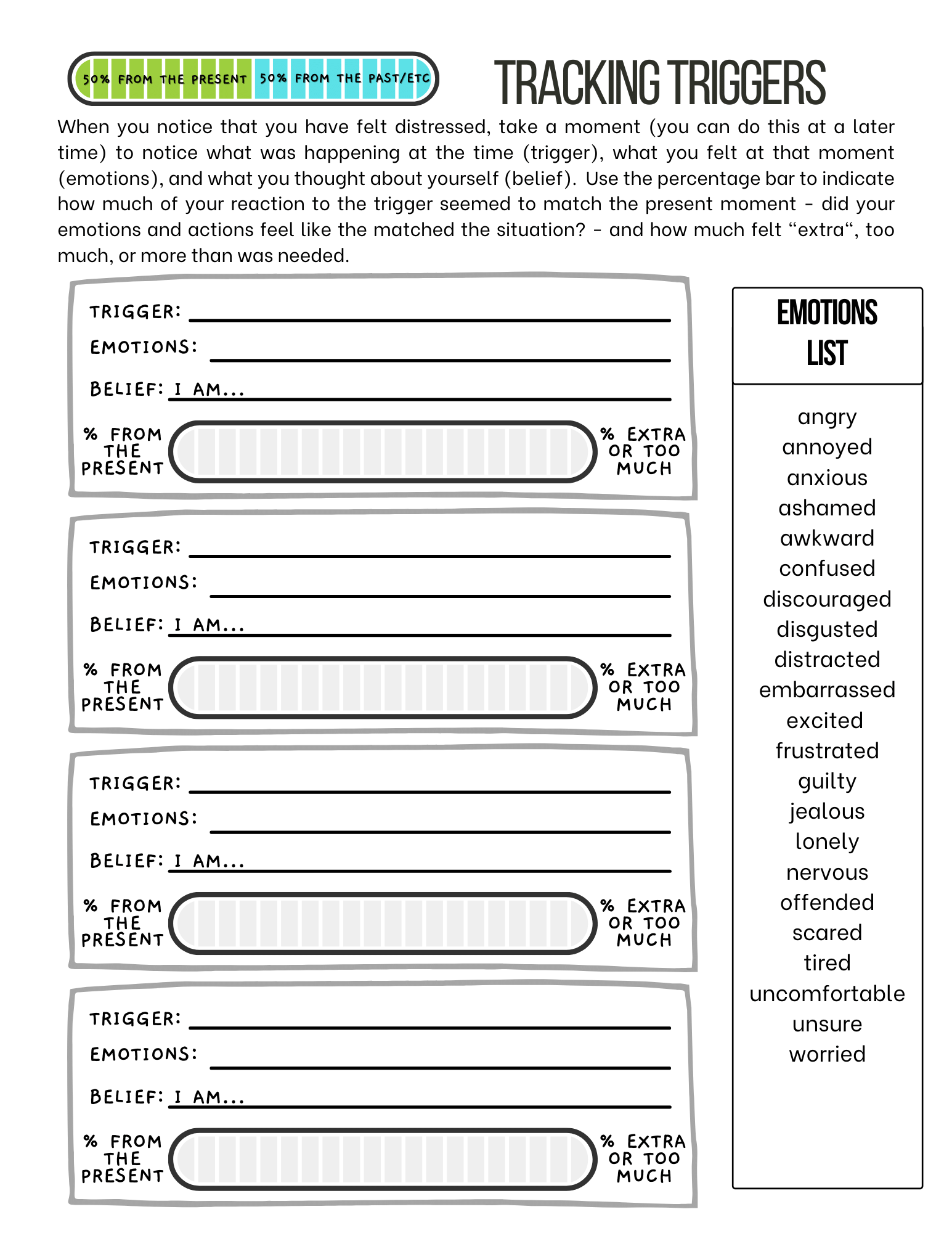
The worksheet below is a resource that we use to help clients notice and track the triggers they have throughout the week. Tracking what triggers your distress can help you understand patterns and possible links to past trauma or stress in your nervous system. This worksheet is especially helpful for those beginning EMDR therapy because it allows you to practice noticing how your thoughts, behaviors, emotions, and body sensations connect in your memory network. An EMDR therapist can help you take these triggers and create a treatment plan to target the memories causing your symptoms. For example, if you notice that you often have anxiety in the grocery store you would write “grocery store” or “shopping” on the Trigger line, then “anxiety”, “fear”, or “nervousness” on the Emotions line, then maybe write a thought that you notice when you think about that trigger and feeling - “I am unsafe” - on the Belief line, and finally when you think about the anxiety that you felt at the store notice how much of that emotion felt like it matched the present moment. If you notice that being in the grocery store was not unsafe and nothing happened in the present that would indicate that you were unsafe in the grocery store, then you might color in only a small sliver of the status bar to show that only a tiny percent of your anxiety seemed to match that situation and the larger percentage of your reaction seemed to be coming from somewhere else (most likely a moment in the past). In your EMDR therapy session, your therapist can help you trace that trigger to a memory in the past (maybe a time when you truly were unsafe in a similar setting or lost in a store as a child). There may be multiple memories related to a trigger in the present. When the memories connected to that anxiety are reprocessed with EMDR therapy, you will notice that your emotions will begin to match the present and you no longer feel anxiety in grocery stores.
Pandemics, such as the 2003 SARS outbreak or Covid-19 which affected the whole world in 2020, wreck havoc with lives and livelihoods. In response, most of the attention becomes focused on those who contract the disease as well as the economic effects. The effects on mental health may not receive as much widespread attention, however they are likely to last well beyond the physical and economic toll.
There are many factors in a pandemic that contribute to its mental health ramifications. In the immediate, it threatens everyone with physical harm and leaves people without a sense of control over their safety. A pandemic also disrupts society at the same level as a terrorist attack or natural disaster, sending waves of anxiety through entire populations. That sense of anxiety is heightened as people live in quarantine arrangements, largely cut off from the community and social support networks which would otherwise help them cope.
Quarantine and social isolation is traumatic enough, however for many it is made even worse by being trapped in living arrangements with an abusive partner or parent. Financial distress and large-scale disasters are known to increase the rates of suicide and self-harm. The long-term economic effects of the coronavirus combined with a breakdown in a community’s ability to connect and respond resiliently may even increase rates of human trafficking.
Unsurprisingly, those hardest hit by the mental and emotional trauma of a pandemic are those personally impacted by death. This includes those who contract the disease and their family members as well as the front-line medical workers who deal with overwhelming caseloads and stressful, evolving work environments. Society owes a special debt of duty to care for the mental health of those doctors, nurses, paramedics, and other medical staff who risk their own well-being to look after the needs of others during a pandemic.
Research and experience tells us that those not directly affected by the illness could also face mental health challenges well after the pandemic has passed. People seriously affected financially as they lose jobs or retirement savings may face ongoing mental health effects. In places put under quarantine during the SARS outbreak, higher levels of depression and PTSD were reported. People who spend a lot of time absorbing traumatic news or social media may also be at a higher risk for later, ongoing mental health concerns.
Hope Roots offers training and resources in body-focused therapies for those who are supporting people affected by traumatic events. Click here to find training for yourself and to learn how you can provide resources to those responding in under-serviced communities. Or, click here to learn about our summer 2020 Henna for Hope Campaign.
1 https://www.psychologytoday.com/us/blog/talking-about-health/202003/mental-health-in-time-pandemic
2 https://www.nationalelfservice.net/mental-health/ptsd/covid-trauma-response/
3 https://polarisproject.org/blog/2020/04/covid-19-may-increase-human-trafficking-in-vulnerable-communities/
4 https://www.psychologytoday.com/us/blog/talking-about-health/202003/mental-health-in-time-pandemic