On November 9th, 2023, Hope Roots hosted a 1-hour Free Discussion with Dorinna Ruh with tools to help therapists learn to assess clients for dissociation. This call, and other training resources are provided as part of Hope Roots' mission to increase access to trauma-informed care. For more resources like this, please subscribe on YouTube at https://www.youtube.com/@hoperoots and signup for email updates when new resources are posted.
Event Description
Discovering a client’s dissociative disorder is the first step toward their receiving proper treatment. Yet many therapists do not get adequate training regarding dissociation, specifically how to assess it. As a result, it takes between 5 - 12 years for someone in therapy to get diagnosed with a dissociative disorder (Brand BL, Loewenstein RJ, Spiegel D. Dispelling myths about dissociative identity disorder treatment: an empirically based approach. Psychiatry. 2014 Summer;77(2):169-89).
Dorinna Ruh has taught advanced EMDR Therapy skills since 2010 as an EMDRIA-approved consultant and specializes in dissociative disorders. Learn more about Dorinna’s work at https://advanced-emdr-education.com/ In this free call, Dorinna will review dissociation assessment for therapists who want to ensure they have the basic skills needed to identify clients who may have a dissociative disorder. No CEUs will be given.
Donations Appreciated
If you find this offering of value, please consider sending a donation to Hope Roots, so we can continue our mission of increasing access to trauma-informed care (including training opportunities like this!). You can also Venmo a donation (@hoperoots).
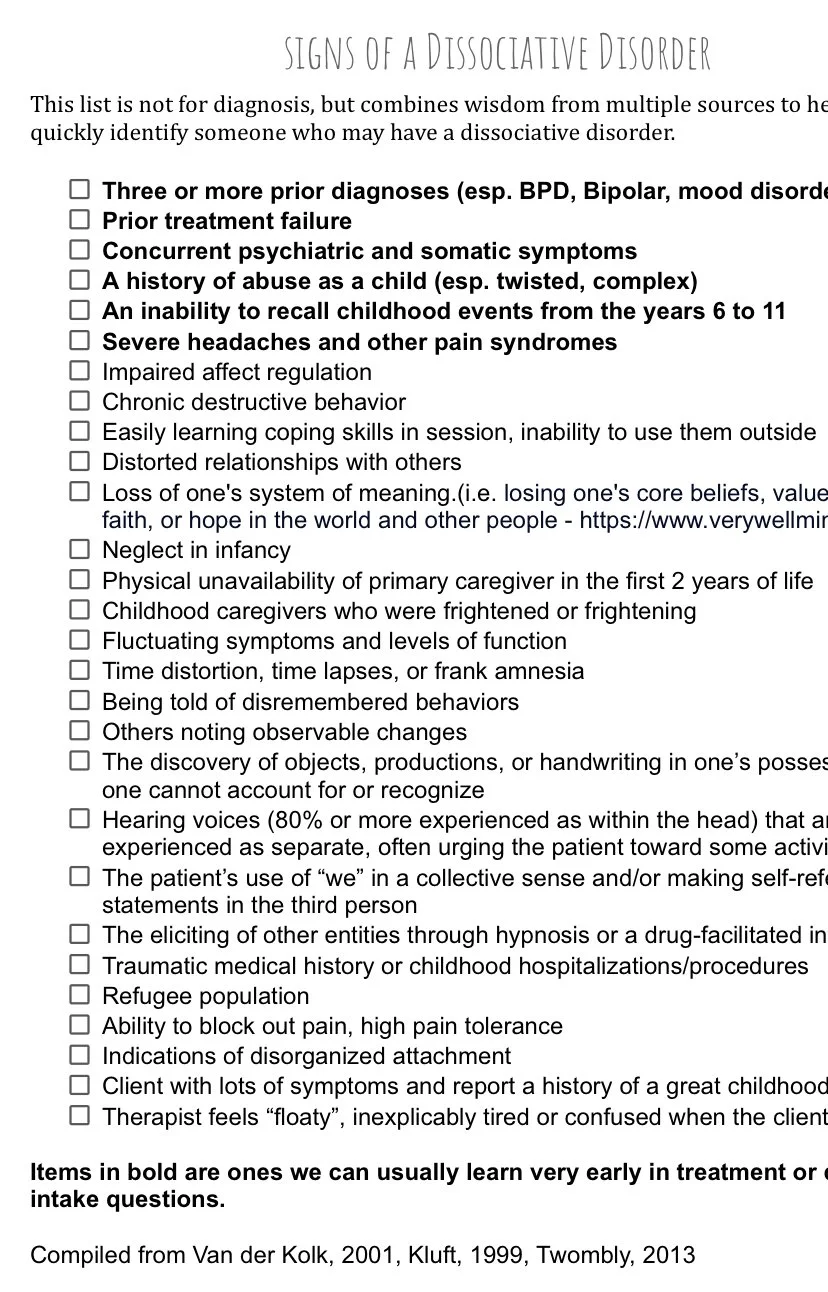
This list is not for diagnosis, but combines wisdom from multiple sources to help trauma therapists more quickly identify someone who may have a dissociative disorder. Click here to download a PDF of this handout.
Three or more prior diagnoses (esp. BPD, Bipolar, mood disorders)
Prior treatment failure
Concurrent psychiatric and somatic symptoms
A history of abuse as a child (esp. twisted, complex)
An inability to recall childhood events from the years 6 to 11
Severe headaches and other pain syndromes
Impaired affect regulation
Chronic destructive behavior
Easily learning coping skills in session, inability to use them outside
Distorted relationships with others
Loss of one's system of meaning.(i.e. losing one's core beliefs, values, religious faith, or hope in the world and other people - https://www.verywellmind.com)
Neglect in infancy
Physical unavailability of primary caregiver in the first 2 years of life
Childhood caregivers who were frightened or frightening
Fluctuating symptoms and levels of function
Time distortion, time lapses, or frank amnesia
Being told of disremembered behaviors
Others noting observable changes
The discovery of objects, productions, or handwriting in one’s possession that one cannot account for or recognize
Hearing voices (80% or more experienced as within the head) that are experienced as separate, often urging the patient toward some activity
The patient’s use of “we” in a collective sense and/or making self-referential statements in the third person
The eliciting of other entities through hypnosis or a drug-facilitated interview
Traumatic medical history or childhood hospitalizations/procedures
Refugee population
Ability to block out pain, high pain tolerance Indications of disorganized attachment
Client with lots of symptoms and report a history of a great childhood
Therapist feels “floaty”, inexplicably tired or confused when the client is present .
Items in bold are ones we can usually learn very early in treatment or during intake questions
Compiled from Van der Kolk, 2001, Kluft, 1999, Twombly, 2013